Through our partnership with the Wyoming Department of Health, Division of Healthcare Financing (Medicaid), we coordinate care and build teams of support through the High Fidelity Wraparound model to manage day-to-day challenges of children, youth and their families where they live.
Our local Magellan Healthcare, Inc. team serves as the Care Management Entity for youth with complex behavioral health conditions. A Care Management Entity manages the High Fidelity Wraparound program. Which means we set the rules and provide training for all the people involved in the High Fidelity Wraparound process.
We know that behavioral health conditions can create challenges in many areas:
- at home
- at school
- in the community
Our method helps children and youth stay connected to his or her family and be successful in school. We help youth:
- develop life skills
- keep ties to their communities
- support good health
- prepare to become adults
We use a family-centered approach. We use local community resources to build a team that understands and respects each family’s:
- unique qualities and culture
- strengths and challenges
We are passionate about what we do and have many agencies and people around the state working on the High Fidelity Wraparound model.
Here is a snapshot of how youth and families and Magellan, the Wyoming Department of Health and provider agencies work together in the High Fidelity Wraparound process:
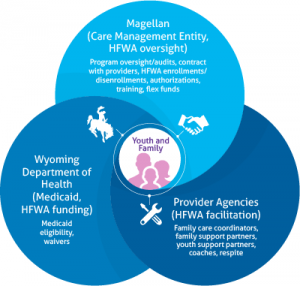
Magellan (Care Management Entity HFWA Oversight)
Program oversight/audits, contract with providers, HFWA enrollments/disenrollments, authorizations, training, flex funds
Wyoming Department of Health (Medicaid HFWA Funding)
Medicaid Eligibility Waivers
Provider Agencies (HFWA Facilitation)
Family Care Coordinators, family support partners, youth support partners, coaches, respite
Wyoming’s High Fidelity Wraparound program is made possible by the Wyoming Department of Health, Division of Healthcare Financing.

